Prednisolone is a synthetically manufactured glucocorticoid medication used to treat a variety of inflammatory and autoimmune conditions. With its potent anti-inflammatory and immunosuppressant properties, prednisolone has become an indispensable medicine in clinical practice today.
In this comprehensive guide, we will cover everything you need to know about prednisolone, including:
What is Prednisolone and How Does it Work?
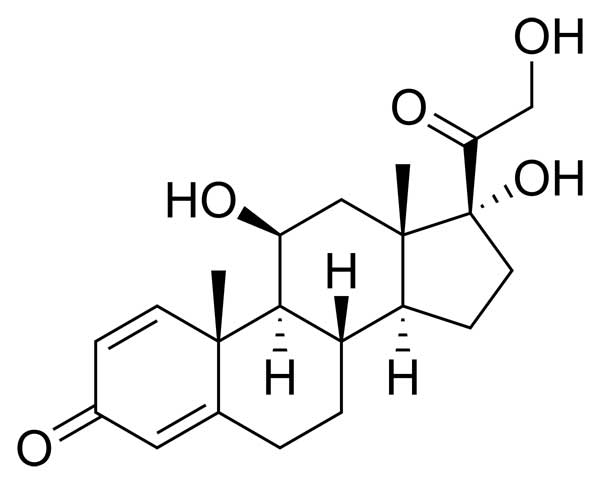
Prednisolone is a synthetic adrenocortical steroid medication, classified as a glucocorticoid. Structurally, it contains a 21-carbon steroid nucleus known as a pregnane, with two double bonds at carbons 1 and 4. It also contains ketone groups at carbons 3 and 20. The chemical name of prednisolone is Pregna-1,4-diene-3,20-dione, 11,17,21-trihydroxy-, reflecting the presence and positions of functional groups on its steroid backbone.
Prednisolone works through multiple mechanisms to potently reduce inflammation and immune activity in the body. It can:
- Increase glucose production by the liver while reducing peripheral glucose uptake, causing hyperglycemia
- Stimulate fat breakdown (lipolysis) and protein catabolism
- Increase uric acid excretion by the kidneys
- Inhibit the activity of inflammatory cells like eosinophils and lymphocytes
At the molecular level, prednisolone readily crosses cell membranes and binds to cytoplasmic glucocorticoid receptors, causing them to dissociate from heat shock protein 90 (Hsp90). The activated glucocorticoid receptors can then translocate into the nucleus, homodimerize, and influence gene transcription. This leads to increased production of anti-inflammatory proteins like annexin A1 and lipocortin-1 while suppressing synthesis of inflammatory cytokines like interleukins and TNF-alpha.
By binding to and inhibiting NF-kB, prednisolone also prevents downstream expression of various inflammatory genes and proteins by immune cells. Collectively, these diverse actions make prednisolone highly effective at combating excessive or abnormal inflammation in tissues.
Clinical Uses of Prednisolone
Some key uses of prednisolone in medicine include treating:
- Inflammatory bowel diseases like ulcerative colitis and Crohn’s disease
- Rheumatoid arthritis, psoriatic arthritis, and other inflammatory joint disorders
- Acute leukemia and certain lymphomas
- Multiple sclerosis
- Severe allergic reactions affecting the skin, eyes, or airways
- Asthma and COPD exacerbations
- Adrenal insufficiency (when given with fludrocortisone)
Typical dosing of prednisolone ranges from 10 mg to 60 mg daily, depending on the condition being treated. For multiple sclerosis flares, doses can reach 200 mg daily over a short period.
Due to its immune-suppressing effects, patients taking prednisolone long-term need to be monitored closely for signs of infection, which may be more likely to develop or get worse with treatment. Fungal infections, reactivation of tuberculosis or chickenpox (varicella zoster), and other opportunistic infections are particular concerns.
Side Effects and Safety Considerations with Prednisolone Therapy
While highly effective, prednisolone does carry some important side effects and risks, especially with longer-term treatment. Potential adverse effects include:
Fluid Retention and High Blood Pressure
The mineralocorticoid activity of prednisolone can lead to sodium and water retention, predisposing patients to edema, congestive heart failure exacerbation, and high blood pressure. This makes monitoring fluid status and electrolytes important.
HPA Axis Suppression
By providing high levels of exogenous glucocorticoid, prednisolone may suppress the body’s own production of cortisol by the adrenal glands. This makes slowly tapering the dose of prednisolone necessary rather than abruptly stopping the drug.
Hyperglycemia and Diabetes Risk
Elevated blood glucose is a predictable effect of prednisolone. Diabetics and pre-diabetics may experience worsening control of their blood sugars while on the medication.
GI Bleeding
Prednisolone can increase the chance of peptic ulcer disease and subsequent bleeding from the stomach or intestines.
Osteoporosis
Decreased bone density is another potential complication of prednisolone therapy, especially in post-menopausal women. Calcium and vitamin D supplementation may be protective.
Cataracts and Glaucoma
Prolonged prednisolone use can increase intraocular pressure and the risk of cataracts or glaucoma. Periodic ophthalmologic exams help detect these complications early.
Key Takeaways About Prednisolone
- Prednisolone is a very versatile anti-inflammatory glucocorticoid medication used for a variety of immune-mediated conditions
- It works by binding to cytoplasmic receptors that then influence gene transcription to reduce inflammation
- Benefits need to be weighed against risks like infection, osteoporosis, cataracts, and diabetes for long-term use
- Tapering the dose gradually prevents complications from HPA axis suppression
- Monitoring for signs of infection, fluid retention, and hyperglycemia is important for patient safety
With proper precautions and monitoring, prednisolone remains an extremely beneficial medicine for controlling problematic inflammation and overactive immune responses. Your physician can determine if prednisolone is appropriate for your situation and provide guidance on minimizing side effects should it be prescribed.
